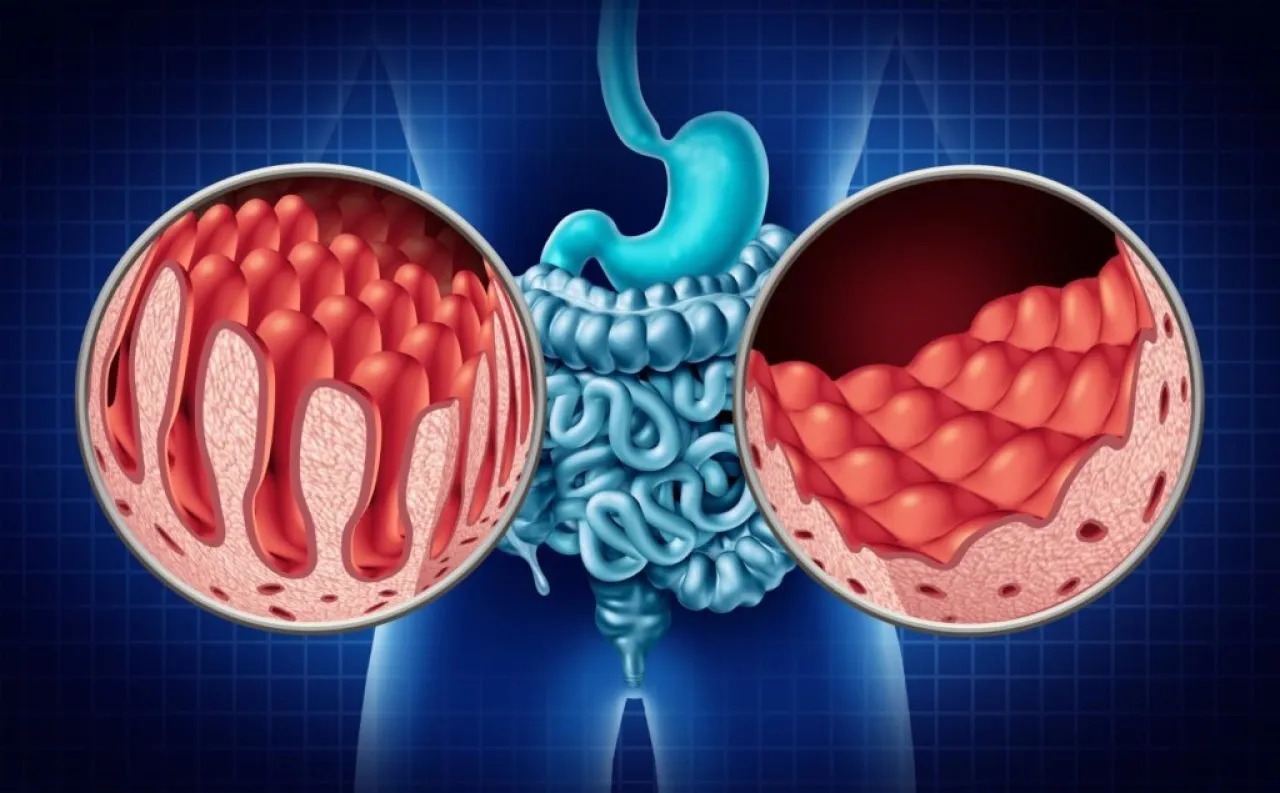
Khaberni - The Family Health Care Institute's bulletin discusses celiac disease today, Tuesday. Celiac disease is a chronic immune disorder marked by an abnormal immune response to gluten, a protein found in wheat and barley. When consumed by individuals with celiac disease, their immune system attacks the lining of their small intestine, leading to inflammation and atrophy of the intestinal villi (tiny finger-like protrusions in the small intestine's lining).
The bulletin clarifies the causes of this disease, its symptoms that may appear in different ways, the necessary tests for diagnosis, as well as possible complications and treatment methods.
The damage caused by celiac disease impairs nutrient absorption and causes a wide range of digestive and non-digestive symptoms. Approximately 1% of the global population is affected by the disease, although many cases remain undiagnosed due to symptom variability. Early identification and proper management are essential for preventing complications and improving quality of life.
** Causes
Celiac disease occurs in individuals with a genetic predisposition, especially those carrying the HLA-DQ2 or HLA-DQ8 genes. While these genes are a cofactor, they alone are not sufficient for contracting the disease. The immune response is triggered when gluten proteins, primarily gliadin, contact the intestinal surface. An enzyme called "tissue transglutaminase (tTG)" in the intestines modifies gliadin to make it more likely to provoke the immune system. This activation leads to the mobilization of T-cells and the release of inflammatory cytokines, eventually resulting in intestinal villi damage over time.
Villous atrophy results in poor nutrient absorption, such as iron, calcium, folic acid, and fat-soluble vitamins. Over time, anemia, osteoporosis, weight loss, neurological disorders, and growth delay in children may manifest. The disease also increases the risk of other immune disorders such as Type 1 diabetes, autoimmune thyroid diseases, and certain liver diseases.
** Symptoms
Celiac disease can manifest in various ways, making its diagnosis challenging. Traditionally, the disease has been associated with digestive symptoms, but many patients present with non-digestive symptoms or may not show clear symptoms at all.
1 - Digestive symptoms
- Chronic diarrhea
- Abdominal pain and bloating
- Malabsorption and weight loss
- Constipation in some cases
- Excessive gas
- Fatty or foul-smelling stools
2 - Non-digestive symptoms
- Anemia due to iron deficiency that does not respond to treatment
- Osteoporosis or reduced bone mass
- General fatigue
- Peripheral neuropathy
- Headaches or migraines
- A skin rash called dermatitis herpetiformis
- Infertility or recurrent miscarriages
- Delayed puberty in adolescents
3 - Symptoms in children
They may exhibit classic malabsorption symptoms such as:
- Growth failure
- Delayed weight and height gain
- Irritability and moodiness
- Abdominal bloating
- Enamel defects in teeth
Due to the variability of symptoms, the disease can be confused with irritable bowel syndrome, lactose intolerance, inflammatory bowel diseases, and others.
** Diagnosis
Diagnosis usually begins with blood tests. The most common test is for antibodies against tissue transglutaminase (tTG-IgA). Total IgA levels are measured to avoid false-negative results due to a lack of IgA; if deficient, IgG-based tests such as DGP-IgG are used.
If the tests are positive, an upper endoscopy is conducted with biopsies from the small intestine, which is the gold standard for diagnosis. Biopsies show villous atrophy and increased lymphocytes. It is important that the patient continues to consume gluten during testing, as cessation may lead to false-negative results.
Genetic testing does not confirm diagnosis but can rule it out if causative genes are absent.
** Treatment: Gluten-free diet
The only proven treatment is a strictly gluten-free diet for life. Avoiding gluten helps heal the intestinal lining, improves symptoms, and reduces complications. Even very small amounts (less than 20 parts per million) can cause damage, so absolute adherence is necessary.
** Foods containing gluten
- Wheat and its derivatives
- Barley
- Many processed foods, sauces, and soups
** Safe foods
- Rice, corn, and quinoa
- Potatoes and legumes
- Fruits and vegetables
- Meats, eggs, and fish
- Gluten-free oats
** Long-term follow-up
Regular follow-up is essential to ensure adherence to the diet and to monitor for complications.
1 - Nutritional monitoring
Includes monitoring levels of:
- Iron
- Vitamin D
- Vitamin B12
- Folic acid
- Calcium
2 - Monitoring associated diseases
Some patients may suffer from:
- Autoimmune thyroid diseases
- Type 1 diabetes
- Skin or liver diseases
3 - Bone health
Bone density measurement is recommended at diagnosis and subsequently as needed.
4 - Non-responsive celiac
Symptoms may persist despite the diet due to:
- Unintended gluten intake (most common)
- Microscopic colitis
- Small intestinal bacterial overgrowth
- Pancreatic insufficiency
In rare cases, refractory celiac appears, requiring specialized therapeutic intervention.
** Complications
Without treatment, the disease can lead to:
- Severe malnutrition
- Osteoporosis
- Neurological disorders
- Infertility and miscarriages
- Growth delay in children
- Increased risk of certain types of cancer such as intestinal lymphoma.