Khaberni - The Family Health Care Institute's newsletter (part of the King Hussein Foundation institutes) discusses today, Tuesday, pharyngitis, which is considered a widespread clinical condition with significant impact on public health and represents a large percentage of upper respiratory infections seen in medical clinics.
The newsletter clarifies the causes of pharyngitis, which are classified into infectious and non-infectious, symptoms and clinical signs, diagnostic procedures and tests, in addition to treatment methods, and the necessary steps for disease prevention.
This disease affects all age groups, but it is more common among school-age children and teenagers. Although most cases are mild and heal spontaneously, the possibility of bacterial complications, misuse of antibiotics, and increased healthcare costs make accurate diagnosis and proper management critical.
The pharynx is located between the nasal cavity and the esophagus, playing a vital role in breathing and swallowing. Inflammation in this area can result from infectious, allergic, environmental factors, or systemic diseases. Distinguishing between viral and bacterial causes is essential, as antibiotic treatment only benefits bacterial cases.
Pharyngitis, commonly known as sore throat, is an inflammatory condition that affects the mucous membrane of the pharynx, leading to throat pain, difficulty swallowing, and a general feeling of discomfort. It is one of the most common reasons for doctor visits and antibiotic prescriptions in both adults and children. Although viral infections represent the majority of cases, bacterial pharyngitis—especially those caused by Group A Streptococcus—requires rapid diagnosis and appropriate treatment to avoid complications. This review aims to provide an updated perspective on pharyngitis, in terms of its causes, symptoms, diagnostic methods, and treatment strategies, with a focus on rational use of antibiotics.
** Causes
Pharyngitis can be classified into infectious and non-infectious based on the cause.
1 - Infectious causes
Viruses cause about 70–90% of pharyngitis cases. Common viruses include:
- Rhinovirus.
- Coronavirus.
- Adenovirus.
- Parainfluenza.
- Influenza virus, Epstein–Barr Virus - EBV.
- Coxsackie Virus.
Typically, viral pharyngitis appears as part of an upper respiratory infection, associated with symptoms such as cough, nasal congestion, conjunctivitis, and hoarseness. Epstein–Barr virus infection often accompanies severe throat inflammation, swollen lymph nodes, and enlarged liver and spleen.
However, bacterial causes are less common but more clinically significant. Group A Streptococcus (Streptococcus pyogenes) is the most important bacterial cause of pharyngitis. Other less common pathogens include: Group C and G streptococci, Mycoplasma pneumoniae, Chlamydia pneumoniae, Neisseria gonorrhoeae, and Corynebacterium diphtheriae.
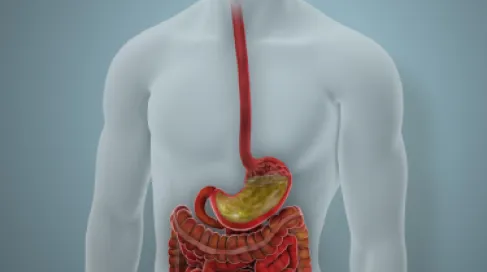
2. Non-infectious causes
Include cases resulting from:
- Allergies (such as dust, pollen, or pets).
- Smoking or air pollution.
- Gastroesophageal reflux disease (GERD).
- Overuse of the voice.
- Dry air or mouth breathing.
These cases are usually chronic or recurrent and not acute.
Pharyngitis results from irritation and inflammation of the mucous membranes due to infection or irritants. In bacterial cases, Group A streptococci produce toxins and enzymes that damage the epithelial tissues, causing swelling, redness, and secretion formation. The immune response contributes to the pain and inflammation by releasing cytokines and recruiting white blood cells.
** Symptoms and clinical signs
The primary symptom is throat pain, often accompanied by difficulty or pain when swallowing.
Other symptoms and signs include:
- Fever and general fatigue
- Redness and swelling in the pharyngeal mucous membrane
- Enlarged tonsils or secretions on them
- Swollen and painful anterior cervical lymph nodes
- Headache and abdominal pain (especially in children)
Viral pharyngitis typically accompanies respiratory symptoms such as coughing, colds, and conjunctivitis,
while Streptococcal pharyngitis (bacterial) is characterized by:
- Sudden onset of throat pain.
- High fever.
- Absence of cough.
- Presence of secretions on the tonsils.
- Hemorrhagic spots on the throat roof.
If bacterial pharyngitis is not treated, it can lead to complications like peritonsillar abscess, rheumatic fever, or post-streptococcal glomerulonephritis.
** Diagnosis
Diagnosis is based on clinical history and physical examination, but as symptoms can be similar between viral and bacterial infections, supportive tests are advised.
Centor Criteria
The Centor system or the modified McIsaac version assesses the probability of streptococcal infection, considering:
- Presence of secretions on the tonsils.
- Swollen painful anterior cervical lymph nodes.
- Temperature > 38°C.
- Absence of cough.
- Patient age.
The higher the points, the greater the likelihood of bacterial infection.
Rapid Antigen Detection Test (RADT)
Detects the presence of streptococcal antigens quickly and with high accuracy within minutes. It has moderate sensitivity and high specificity. If the result is negative in children with symptoms, a throat culture is recommended for confirmation.
Throat culture
Considered the gold standard for diagnosis, it has a sensitivity of 95% and specificity of 100%, but it requires 24 to 48 hours to show results.
Additional tests
In cases of suspected infectious mononucleosis, heterophile antibody tests or EBV tests are conducted, while cases suspected of gonococcal or diphtheria infections require specific cultures.
** Treatment
1. Supportive treatment
Most viral cases heal spontaneously within a week, and treatment aims to alleviate symptoms:
- Increasing fluids and rest
- Gargling with warm salt water
- Using pain relievers like paracetamol or ibuprofen
- Throat lozenges or sprays to relieve pain
Antibiotics are not used in viral cases.
2. Antibiotic treatment
Used only in confirmed or highly suspected cases of streptococcal pharyngitis. It aims to shorten symptom duration, prevent infection spread to contacts, and avoid complications.
Recommended treatments:
- Penicillin V: 250 mg four times daily or 500 mg twice daily for 10 days
- Amoxicillin: a dose of 50 mg/kg once daily (maximum 1 g) for 10 days
For those allergic to penicillin:
- Alternatives like cephalexin, azithromycin, or clindamycin can be used.
Patients must complete the full course of treatment even if symptoms improve early.
3. Managing complications
Potential complications include:
- Peritonsillar abscess: treated with surgical drainage and intravenous antibiotics
- Rheumatic fever: can be prevented by early treatment
- Post-streptococcal glomerulonephritis: treated supportively
** Prevention
Prevention strategies include:
- Regular hand washing and following cough and sneeze etiquette.
- Avoiding direct contact with infected individuals.
- Cleaning shared tools and surfaces.
- Covering the mouth and nose when coughing or sneezing.
Persons with streptococcal pharyngitis are advised to stay home for at least 24 hours after starting antibiotic treatment to reduce infection spread to others.