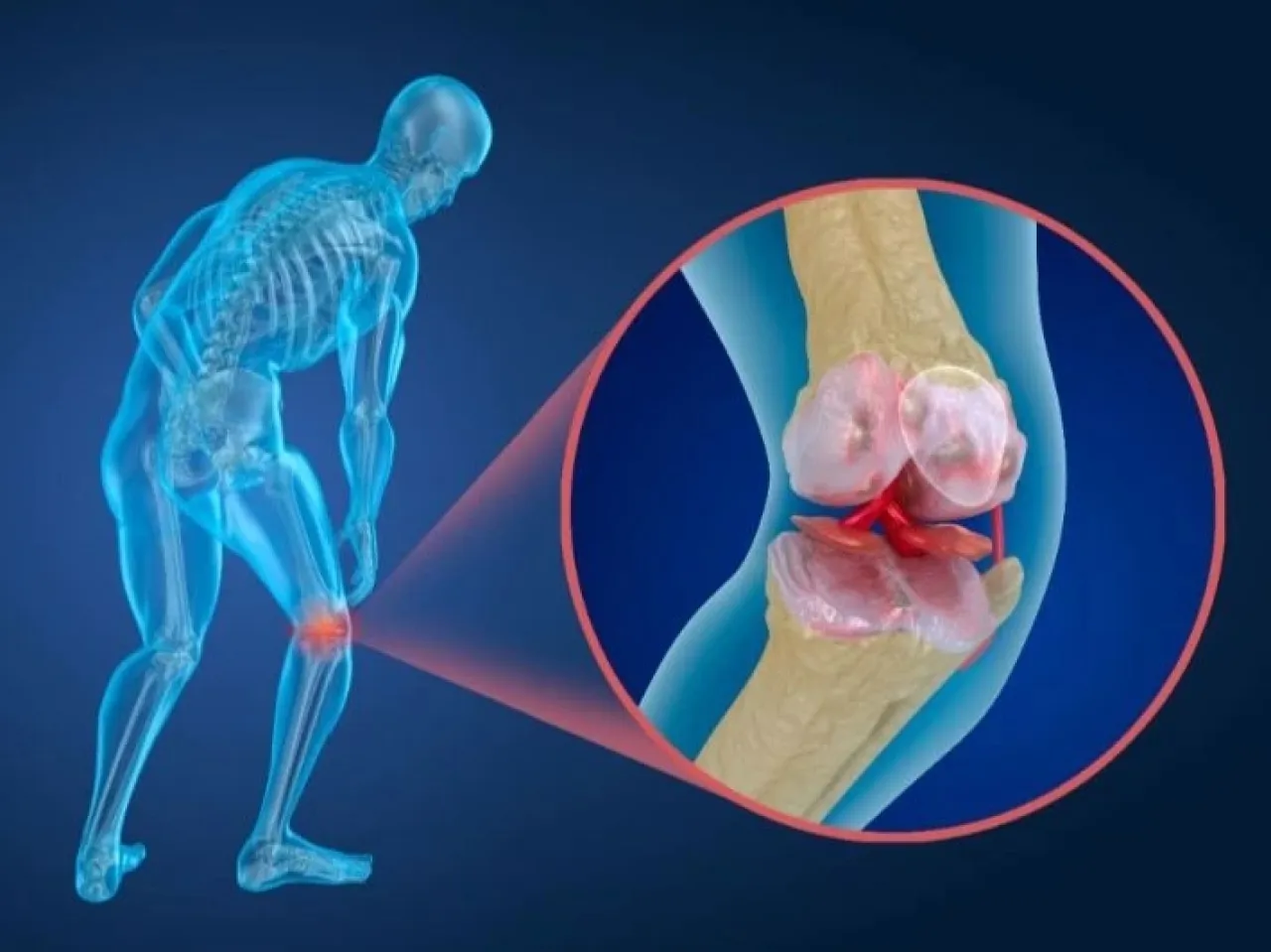
Khaberni - Joint arthritis is a condition that causes the joints to become stiff and cause a lot of pain, and the most important symptoms of joint arthritis are joint pain and stiffness. Some people also suffer from swelling and the sounds of creaking or clicking when moving the affected joints. Join us through the following article to learn about the current methods used in treating joint arthritis and minimizing it as much as possible, and whether there is a permanent cure for this condition or not.
Is there a permanent treatment for joint arthritis?
There is no permanent cure for joint arthritis, but the condition does not necessarily worsen over time, and there are a number of treatments available to help alleviate symptoms.
The main treatments for joint arthritis include:
• Lifestyle measures, such as maintaining a healthy weight and regularly exercising.
• Medications to relieve pain.
• Supportive therapies, to help make daily activities easier.
• In rare cases, if other treatments are not helpful, surgery can also be performed to repair, reinforce, or replace damaged joints.
Treating Joint Arthritis and Lifestyle Changes
Exercises
Exercise is one of the most important ways to treat joint arthritis regardless of your age or physical fitness level. Your physical activity should include a mix of exercises to strengthen your muscles and general fitness improving exercises.
If joint arthritis causes pain and stiffness in your body, you might think that exercise will exacerbate your symptoms. However, regular exercise that keeps you active and builds muscles and strengthens joints usually helps improve symptoms and relieve them.
Exercise is also beneficial for losing weight and improving your posture and reducing stress, all of which will alleviate symptoms.
Your general practitioner, or perhaps a physiotherapist, will discuss with you the benefits you can expect from an exercise program and can provide you with a home exercise plan. It is important to follow this plan because there is a risk that too much exercise too quickly or performing the wrong exercises could damage your joints rather than treat joint arthritis or reduce it.
Losing Weight
Being overweight or obese increases the harshness of joint arthritis because it can put some of your joints under increased pressure.
If you are overweight, try losing weight by doing more physical activity and eating a healthy diet.
Discuss any new exercise plan with your doctor or physiotherapist before starting. They can assist in designing an appropriate exercise program for you, and your doctor can provide advice on how to lose weight slowly and safely.
Treating Joint Arthritis with Medications
Your doctor will talk to you about the medications that can manage the symptoms of joint arthritis, including pain relievers. Sometimes, a combination of treatments, medications, assistive devices, or surgery, may be needed to help control your pain.
Pain Relievers
The type of pain reliever your doctor may recommend for you depends on the severity of the pain and other conditions or health issues you may have. The main medications used include:
Paracetamol
If you suffer from pain caused by arthritis, your doctor may initially suggest taking paracetamol. This is available over-the-counter at pharmacies. It's best to take it regularly rather than waiting until the pain becomes unbearable.
However, always follow the dose recommended by your doctor and do not exceed the maximum dose indicated on the package.
Non-Steroidal Anti-Inflammatory Drugs (NSAIDs)
If paracetamol does not effectively control the pain of osteoarthritis (joint arthritis), your general practitioner may prescribe a stronger pain reliever. Non-steroidal anti-inflammatory drugs are pain relievers that work by reducing inflammation.
There are two types of NSAIDs, which work in slightly different ways:
• Traditional NSAIDs, such as ibuprofen, naproxen, or diclofenac.
• COX-2 inhibitors, commonly called coxibs like celecoxib and etoricoxib.
Some NSAIDs are available as creams (topical NSAIDs) that are applied directly to the affected joints.
Some topical NSAIDs are available over-the-counter, and can be particularly effective if you suffer from arthritis or joint arthritis in your knees or hands. In addition to helping to relieve pain, they can also help reduce any swelling in your joints.
Your doctor will discuss with you which type of NSAIDs you should take and the benefits and risks associated with them.
Side Effects of NSAIDs
NSAID tablets may not be suitable for people who have certain conditions, such as asthma, digestive ulcers or angina, or if you have had a heart attack or stroke. And if you're taking low-dose aspirin, ask your doctor whether you should use NSAIDs.
If your doctor prescribes NSAIDs that should be taken orally, they will usually also prescribe a drug called a proton pump inhibitor (PPI) to take at the same time. NSAIDs can break down the stomach lining μâfo that protects it from stomach acid. This drug reduces the amount of acid produced by your stomach, reducing the risk of damage to the stomach lining.
COX-2 drugs have a lower risk of causing stomach issues, but there is still a need to use them with a PPI if you are taking them regularly.
Opioids
Opioids, such as codeine, are another type of pain reliever that may relieve your pain if paracetamol is not effective enough, although opioids do not help treat joint arthritis but can help relieve severe pain, but they can also cause side effects such as drowsiness, nausea, and constipation.
Codeine can be found in combination with paracetamol in common preparations like co-codamol.
Other opioids that may be prescribed for arthritis include tramadol and hydrocodone. Both come in tablet form and as injections.
Tramadol is not suitable if you suffer from uncontrolled epilepsy, and dihydrocodeine should not be used by patients suffering from chronic obstructive pulmonary disease (COPD).
If you need to take opioids regularly, your doctor may prescribe a laxative to take with these medications to prevent constipation.
Capsaicin Cream
Your doctor may prescribe capsaicin cream if you have arthritis in your hands or knees and topical NSAIDs have not been effective in relieving pain.
Capsaicin cream works by blocking nerves that send pain messages in the treated area. You may need to use it for a while before it starts to work. You will experience some pain during the first two weeks of using the cream, but the treatment may take up to a full month.
Apply a pea-sized amount of the cream to the affected joints up to 4 times a day, but keep a gap of 4 hours or more between each application. Do not use capsaicin cream on cracked or inflamed skin and always wash your hands after application.
Be careful not to apply capsaicin cream to sensitive areas, such as your eyes, mouth, nose, and genitals. The cream is made from hot peppers, so if applied to sensitive areas of your body, it is likely to be very painful for a few hours. However, it will not cause any damage.
You may notice a burning sensation on your skin after applying capsaicin cream. There is no need to worry, the more you use it, the less this sensation will be. But avoid using too much cream or bathing with hot water before or after application, as this may increase the burning sensation.
Steroid Injections and Treating Joint Arthritis
Steroids or steroid injections are a type of medication that contains human-made copies of the cortisol hormone, and they are sometimes used in treating particularly painful muscle and bone issues such as joint arthritis and inflammation.
Some people with joint arthritis may be given steroid injections when other treatments are not working. These are injected directly into the affected area; you may first receive a local anesthetic to numb the area and relieve pain.
Steroid injections likely only provide short-term relief. If steroid injections help, up to 3 injections may be given in the same area, with about 3 to 6 months between each treatment session at a minimum.
Treating Joint Arthritis with Plasma Injections
Platelet-rich plasma (PRP) is a new treatment that can be offered to treat all types of arthritis.
PRP is blood plasma containing concentrated platelets that your body uses to repair damaged tissues. Plasma injections have been proven to accelerate the healing process for some people, but their long-term effectiveness is not yet known.
The doctor will take a blood sample from you and place it in a machine; this device separates the platelet-rich plasma from the other components so it can be taken and injected into the affected joints. The injection process usually takes about 15 minutes.
Treating Joint Arthritis and Supportive Therapies
In addition to lifestyle changes and medications, you may also benefit from types of supportive therapy for joint arthritis that can help ease pain and make daily tasks easier.
Transcutaneous Electrical Nerve Stimulation (TENS)
Transcutaneous Electrical Nerve Stimulation (TENS) uses a machine that sends electrical pulses through electrodes connected to your skin. This may help relieve pain caused by osteoarthritis (which includes joint arthritis) by numbing the nerve endings in the spinal cord that control pain.
Treatment for joint arthritis using TENS is usually arranged by a physical therapist, who can advise on the strength of the therapeutic pulses and how long the treatment should continue.
Hot and Cold Compresses
Applying hot or cold compresses to the joints can relieve the pain and symptoms of joint arthritis for some people. Applying hot or cold compresses (depending on your condition) to the affected area can be very effective in alleviating pain.
Special bags are now also available in pharmacies that can be cooled in the refrigerator or heated in a microwave, and work in a similar way.
Treating_JOCDrunks with Manual Therapy
Not using your joints can lead to muscle wastage and may increase joint stiffness. Manual therapy is provided by a physical therapist, who uses stretching techniques to maintain joint flexibility.
Assistive Devices in Treating Joint Arthritis
If joint arthritis is causing mobility problems or difficulty performing daily tasks, several devices can help address these issues. Your doctor may refer you to a physical therapist for specialist help and advice.
If you have joint arthritis in your lower limbs, such as hips, knees, or feet, a physical therapist or occupational therapist may recommend special shoes or insoles for your shoes.
Shoes with shock-absorbing soles can help to alleviate some of the pressure on your leg joints while walking. Special insoles can help spread your weight more evenly and leg supports also work in the same way.
And if you have inflammation in your hip or knee affecting your movement, you may need to use a walking aid, such as a cane. Hold it on the opposite side of your body to your injured leg so that it takes some of your weight.
A brace (a piece of stiff material used to support a joint or bone) may also be helpful if you need to provide some relief for joint pain. A physical therapist can provide you with a brace and offer advice on how to use it correctly.
And if your hands are affected by osteoarthritis, you may also need help with manual tasks, such as operating a tap. Special devices that operate the tap without using your joint can make performing these tasks much easier. An occupational therapist can provide assistance and advice on using assistive devices in your home or workplace.
Are surgeries suitable for treating joint arthritis?
Surgical intervention to treat osteoarthritis is only necessary in a few cases where other treatments were not effective or in cases where one of your joints is severely damaged.
If you need surgery, your doctor will refer you to an orthopedic surgeon. Surgical intervention for osteoarthritis can greatly improve your symptoms. However, undergoing surgery does not guarantee complete symptom relief, and you may still feel pain and stiffness in some cases.
There are several different types of surgery for arthritis. Here are some of the main types of surgery that are performed:
Joint Replacement
Joint replacement surgery is performed to replace the hip and knee joints.
During the procedure, your surgeon will remove the damaged joint and replace it with an artificial joint (prosthesis) made of plastic and metal. The artificial joint can last up to 20 years, although it may eventually need to be replaced.
There is also a new type of joint replacement surgery that uses only metal components and may be more suitable for younger patients with joint arthritis. Your surgeon will discuss with you which type of surgery would be best relative to your condition.
Joint Fusion
If joint replacement for treating joint arthritis is not suitable for you, your surgeon might suggest a procedure known as joint fusion, which permanently fuses the joint.
This means your joint will be much stronger and less painful, although you will not be able to move it.
Osteotomy
If you suffer from arthritis and joint arthritis in your knees but are not suitable for knee replacement surgery, you may be able to undergo a surgical procedure called an osteotomy.
This involves your surgeon adding or removing a small piece of bone either above or below your knee joint. This helps to realign your knee so your weight is not focused on the damaged part of your knee. This procedure can relieve symptoms of joint arthritis, although you may still need knee replacement surgery eventually.
In the end, the methods to treat joint arthritis or at least reduce its pain are numerous, all you have to do is sit down with your doctor and choose the types of treatments that are optimal for your current condition.